Click here to learn and explore more on Healthcare Rehabilitation blog
In this blog you will gain knowledge about various signs and symptoms of lumbar spinal nerve (traversing or exiting nerve root) compression and signs related to impingement or injury of lower limb peripheral nerves.
Let us first have a brief introduction to localization of spinal cord lesion. Having this knowledge is essential during evaluation process in spinal cord injury cases. Also gaining knowledge about peripheral nerve impingement or injury signs will help therapist in differentiating between spinal nerve compression vs. peripheral nerve impingement signs.
Localization of Spinal Cord Lesion :
The affected level (below which the patient has sensory, motor or reflex abnormalities and level above which sensory, motor and reflex function is normal) is the hallmark of spinal cord disease.
First let us appreciate relationship of vertebrae with respect to the spinal cord segment. Calculating the cord level :
- For cervical vertebra : Add 1 (C1 to T1 cord segments)
- For T1-T6 vertebra : Add 2 (T2 to T8 cord segments)
- For T6-T9 vertebra : Add 3 (T9 to T12 cord segments)
- T10 vertebra corresponds to L1-L2 cord segments
- T11 vertebra corresponds to L3-L4 cord segments
- T12 vertebra corresponds to L5 cord segment
- L1 vertebra overlies sacral and coccygeal segments
Level of the lesion : a lesion above the L1 vertebral body may damage both the cord and its roots. Below this, only roots are damaged. Features suggestive of involvement of spinal cord are :
- Presence of sensory deficit and/or motor weakness in both lower limbs and/or upper limbs.
- Bladder and bowel involvement.
- Brown-Sequard syndrome.
- Presence of definite sensory level.
- Root involvement causes severe, sharp, shooting, burning pain radiating into the cutaneous distribution or muscle group supplied by the root; aggravated by movement, straining or coughing.
- Segmental involvement causes continuous, deep aching pain radiating into whole leg or half of body; not affected by movement.
- Root damage signs : lower motor neuron (L.M.N) and sensory impairment appropriate to the distribution of the damaged root.
- Segmental damage signs : L.M.N and sensory impairment appropriate to segmental level. Interruption of ascending sensory and descending motor tracts produces sensory impairment and upper motor neuron (U.M.N) deficit below the level of lesion.
- Lesion within the cord (intramedullary) produces only segmental signs and symptoms.
Despite producing UMN damage, a rapidly progressive cord lesion (acute insult) often produces a 'flaccid paralysis' with loss of reflexes and absent plantar responses. This state is akin to 'spinal shock' seen following trauma. Several days or weeks may elapse before tone returns accompanied by the expected UMN signs.
In subacute or chronic spinal cord pathology, there is a gradual replacement of descending facilitatory influence at the level of dorsal root results in slow developing spasticity without an intervening phase of hypotonia and hyporeflexia. Paraplegia in extension and further leading to paraplegia in flexion.
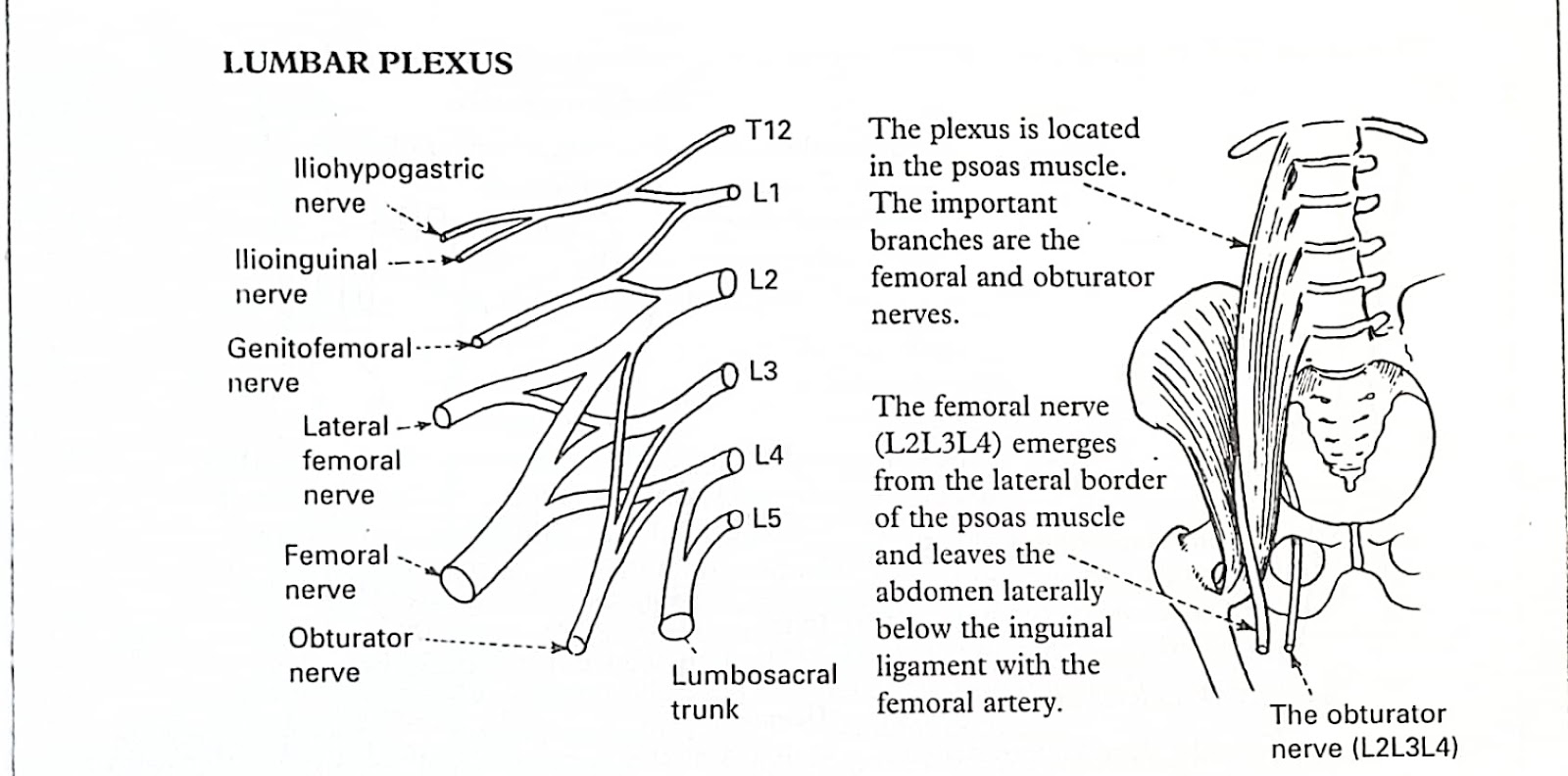
Lower limb plexus lesion :
Upper plexus (Lumbar plexus) lesions produce : Weakness of hip flexion and adduction with anterior leg sensory loss. Femoral nerve and obturator nerve forms the main nerves of lumbar plexus.
Lower plexus (Sacral Plexus) lesions produce : Weakness of posterior thigh (hamstring) and foot muscles with posterior leg sensory loss. Sciatic nerve which is a combination for common peroneal nerve and tibial nerve forms the main nerves of sacral plexus.
Lower limb mononeuropathies :
FEMORAL NERVE (L2L3L4) :
Innervates iliopsoas, sartorius, rectus femoris, pectineus, vastus lateralis, vastus medialis.
Damaged by :
- Fractures of the upper femur
- Congenital dislocation of the hip, hip surgery
- Neoplastic infiltration
- Psoas muscle abscess
- Haematoma into iliopsoas muscle
- Systemic causes of the mononeuropathy e.g. diabetes.
- Weakness of hip flexion.
- Weakness of knee extension with wasting 9f thigh muscles.
- Sensory loss over the anterior and medical aspect of the thigh.
- The knee jerk is lost.
- Same process as the femoral nerve
- During labour and occasionally as a consequence of compression by hernia in the obturator canal
- Weakness of hip extensor rotation and adduction.
- The patient may complain of inability to cross the affected leg on the other.
- Sensory loss is confined to the innermost aspect of thigh.
- The adductor reflex is absent (adductor response to striking the medial epicondyle).
- Congenital or traumatic hip dislocation.
- Penetrating injuries
- Accidental damage from 'misplaced' intramuscular injection.
- Entrapment at sciatic notch.
- Systemic cause of mononeuropathy.
- Weakness of hamstrings muscles with loss of knee flexion.
- Distal foot and leg muscles are also affected.
- Sensory loss involves the outer aspect of leg.
- The ankle reflex is absent.
- Trauma to the head of the fibula (pressure here from kneeling, crossing legs.
- Systemic causes of mononeuropathy, e.g. diabetes.
- Weakness of dorsiflexion and eversion of the foot. The patient walks with a 'foot drop'.
- Sensory loss involves the dorsum and outer aspect of the foot.
- Partial common peroneal nerve palsies are common with very selective muscle weakness.
- Trauma in the popliteal fossa due to fracture of the tibia.
- Systemic causes of mononeuropathy.
- Weakness of plantar flexion and inversion of the foot.
- The patient cannot stand on the toes.
- Sensory loss involves the sole of the foot.
- The ankle reflex is lost.




Comments