➡️ Click here to learn and explore more topics on Healthcare Rehabilitation blog
Cerebral Palsy (CP) is a non-progressive conditions that encompasses neurological, motor and postural deficits. CP is a birth injury of the brain that causes irreversible upper motor neuron disorder. In previous blog we had learned about categories of CP and its features (click on the below link) : https://otpthealthcarerehab.blogspot.com/2020/10/cerebral-palsy-introduction-and.html
Today you will get to know, how persistence of primitive reflexes in CP child hampers their functional motor development. We will also have a brief understanding of interventions that should be aimed for a CP child.
CP is caused by congenital injury or disease at or before birth, acquired due to trauma or haemorrhage or CNS infection or hypoxia. Severity of the CP condition can be assessed using Gross Motor Function Classification System (GMFCS) for gross motor function, Manual Ability Classification System (MACS) for hand function abilities, Communication Function Classification System (CFCS) to assess effectiveness of communication between CP child (sender person) and receiver person of information.
CP child shows characteristic features like :
- retention of primitive reflexes,
- abnormal/variable tone,
- hyperresponsive tendon reflexes (spastic tone),
- asymmetric use of extremities,
- clonus,
- poor feeding amd tongue control,
- involuntary movements (dystonic or choreoathetoid CP)
- Musculoskeletal disorders and deformities develops later when the child is not treated at the earlier stage.
- Visual impairments: Dyskinetic strabismus, more severe gaze dysfunction, optic neuropathy, and cerebral visual impairment, nystagmus (reflexive back and forth movement of eye when head moves).
- Hearing problems occur in approximately 30% to 40% of children with CP. Conductive and sensori-neural impairments are found in children with CP, who should be screened by an audiologist.
- Oral motor impairments namely problems with feeding, swallowing, drooling is present. Gastroesophageal reflux disease (GERD) is common among CP. This can lead to malnourishment in CP child.
- Speech impairments are common in child with CP. They have difficulty in controlling the oral muscles used for speech (lips, tongue, vocal folds, diaphragm, facial muscles), dysarthria (difficulty pronouncing or articulating words), apraxia of speech.
- Cognitive and intellectual impairments : Cognitive deficits tend to be most prevalent and severe in those with spastic tetraplegia, although children with spastic tetraplegia may have normal to near-normal intelligence. In general, patients with more severe neuromuscular impairments are at greater risk for cognitive impairments, but some patients with severe motor impairments can have normal cognition.
- Epilepsy is common in individuals with CP. It is particularly common in those with tetraplegic CP and in those with hemiplegic CP. Partial epilepsy is the most common form of seizure activity in all children with CP, and is especially common in children with hemiplegia who have seizures with a prevalence of around 70% in this specific population. Generalized tonic-clonic seizures are more common in those individuals with spastic tetraplegia and diplegia.
- A wide variety of behavior and emotional disorders are possible, including attention deficit disorder, passivity, immaturity, anger, sadness, impulsivity, emotional lability, low self-esteem, and anxiety. Difficulty with peer relationships has been found even in children with milder CP (GMFCS I). Compared to their classmates, children with mild CP were found to have fewer reciprocated friendships, fewer sociable and leadership behaviors, and were more isolated and victimized by their classmates.
- Decreased bone mineral density (BMD) and increased risk of fracture with minimal trauma is common in patients with moderate to severe CP, especially those who are nonambulatory. By the age of 10 years, most nonambulatory children have osteopenia, as defined by BMD z score of <–2.0 in their femur.
- Lack of development of body symmetry which is normally established by 4 months.
- The head with lack of midline orientation due to deviation of head to the side. This interrupts with the child's ability to orient the hands together in midline and to bring hands towards the mouth.
- Asymmetry may also be noted in the trunk and of it persists then it can lead to scoliosis. The concavity in spine will appear on the side with increased extensor tone and convexity on the side with increased flexor tone.
- The lower jaw will deviate laterally to the side of increased extensor tone which is characteristic of pathological influence of the ATNR and its abnormal affect on the body symmetry.
- Feeding problems will result as upper and lower lips and teeth will not be positioned and aligned properly during feeding.
- Difficulty is visual horizontal tracking across midline.
- Abnormally increased and persistent postural tone (due to affect of dominant ATNR) will prevent the development of Labyrinthine righting reaction, equilibrium and protective extension reaction, which are necessary for normal body and brain growth and development.
- There is severe hyperextension of head and trunk, shoulder girdle retracted with shoulder externally rotated and abducted and elbow flexed with fisted hand. Lower extremities strongly extended at hip and knee with legs internally rotated and adducted. Ankle are plantarflexed with inversion.
- Child may not be able to right or flex the head forward in supine.
- Increased abnormal tone inhibits rotation and the child may not be able to rotate from supine to prone or assume sitting or any higher developmental position.
- Most likely the arms can't be brought forward and oriented midline, nor the hands can't be brought to the mouth.
- Normal postural reflex mechanism are absent.
- Respiration and feeding will also be affect. CP child has to take more efforts to voluntarily control and initiate the feeding task.
- The head is flexed, shoulder girdle protracted, arms tightly flexed and adducted against chest, hands are frequently fisted with thumb adducted across the palm of the hands. Lower extremities are also adducted and flexed at hip and knee and is positioned under abdomen. Sometime extensor tone may dominate flexor tone in lower extremity.
- Child will have difficulty in turning his head from side to side, difficulty in righting the head against gravity in prone position.
- It will also inhibit or interrupt the progression of baby in the developmental prone sequences i.e. weight bearing on forearms, to weight bearing in extended elbows with hands open, to quadruped position, to kneeling position, to half kneeling position, to standing.
- Rotation within the body axis will be inhibited and thus prevent rolling segmentally from prone to supine or assuming prone to sitting position.
- Prehension pattern will be impossible due to fisted hand and adducted thumb across the palm.
- Normal postural reflex reaction mechanisms (protective extension, equilibrium reactions, labyrinthine righting reactions, symmetric tonic neck reflex) are abnormal or hypertonic or not developed.
- Try to maintain and develop symmetric handling techniques, positioning and play activites for CP child : Bilateral arm training or Bimanual training approach is effective in improving coordination between both side and improve hand function. Symmetrical activities involves both the upper limbs to work simultaneous and/or parallel to eachother. This will help to prevent asymmetries in movements or body posture, will limit the influence of abnormal primitive reflexes, will enhance functional use of both affected and non-affected limbs, will improve midline orientation and facilitate development of body.
- Built up parent and child's interest in exercise activities through play. According to Motor relearning principles, interactive and active participation in task, feedback, and practice of functional activities is essential for neurological development and skills aquisition. Modified Constrained Induced Movement Therapy (mCIMT), for hemiplegia CP, should be performed using Motor learning principles approach.
- Focus on developing head control initially. Head control is needed for eye-hand coordination during activities, for tracking and scanning of the environment and receiving information from the environment via visual inputs. In a developing infant, tone in the extremities and trunk is mostly influenced by the neck movement and position untill CNS matures and cortical control is attained.
- Midline orienting play activites and exercises mostly preferred. Sidelying position on wedge or pillow is excellent position for normalization of tone, midline visual hand activities and integrating ATNR. Make use of low technology aids like therapy ball, wedge, bolster for therapy. Depending upon which ADL activity is being performed by the CP child, ensure that the body is placed in correct postural alignment
- Intervention should be different for spastic CP and Athetoid CP with low tone. Influence the amount of postural tone by increasing, decreasing the tone of the CP child. Use of traditional neurophysiological approaches namely neurodevelopment techniques, Proprioceptive Neuromuscular Facilitation, Rood's techniques, Sensory Integration.
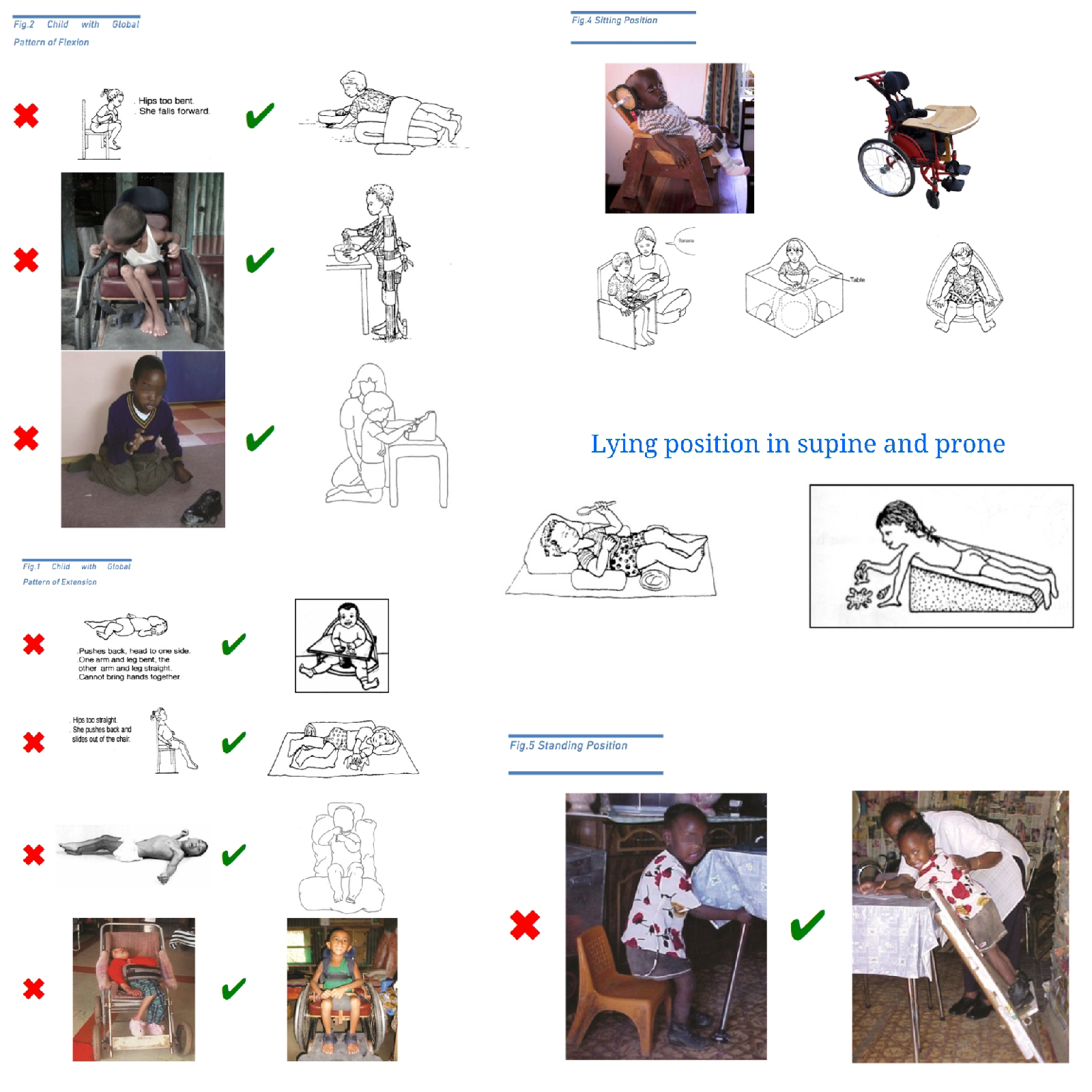
- Inhibiting abnormal movement pattern and posture by implementing midline orienting and symmetric activites, applying traditional approaches (NDT, PNF, SI, Rood's approaches). Always implement and facilitate anti-deformity positions while performing any ADL activity whether in sitting, supine, prone and sidelying position. For example, when sitting on a wheelchair or CP chair the design of the chair should be with respect to the CP child conditions. Neural alignment and appropriate posture of the body should be maintained during activities of feeding, dressing, eating, bathing, writing, walking etc.
- For choreoathetoid or athetoid and Ataxic CP : Focus on co-contractions of joint to decrease uncontrolled movement pattern. Athetosis which refers to fluctuating muscle tone and there is no adequate co-contractions of the proximal and distal joints, which is necessary for stability, mobility and postural control. Focus on the weight bearing patterns and strengthening of joint through play and functional activities to improve control and selective movement pattern.
- For Spastic CP : Focus on improving and increasing the freedom of movements and avoiding sustained abnormal positioning to prevent contractures. Spastic CP has hypertonia and constant co-contractions of the agonist and antagonist muscles which inhibits any type of relaxation when awake or asleep. This will increase the vulnerability of developing abnormal body postures and contracture.
- Facilitation of normal responses : Reflex integration exercises for abnormally present primitive reflexes should to taught first. Then facilitate postural reflex like protective extension, equilibrium reactions, optical and labyrinthine righting reactions using various low cost rehabilitation aids. This will improve neuronal brain maturation, provides foundation for all purposeful movements and skill to be performed. This also improves and assists in stability, mobility and controlled mobility patterns. Therapy can be done using developmental sequence pattern by considering developmental motor milestones.
- Remediation of the feeding problems should be done using appropriate positioning, improving jaw control (manually by mother), desensitizing oral tactile defensiveness, adapted drinking using various device, spoon feeding, facilitate chewing and drooling control techniques.
- Cognitive Orientation to Daily Occupational performance (CO-OP) approach for cognitively oriented CP child. This approach can be suitable for CP children or adolescent who has sufficient cognitive abilities to think, interact with therapist and discover their own strategies to achieve a goal. For example, the goal can be improving handwriting, tying shoelace, wearing a shirt. Leisure goal can include walking outdoor with family, riding cycle, playing ball catching and throwing. The CO-OP approach is a child centred, performance based, problem-solving approach that enables skill acquisition through the process of strategy use and guided discovery.
- Educational approach for creating and increasing awareness and social support for CP child and his/her parents. Adaptation and environmental modifications approach for the family should be taught. Prescribe hand splints and lower limb orthosis to prevent contractures and to keep the hand and lower limbs in functional alignment and working. Stress Management for CP child, who has good cognition and IQ, with only motor deficits.
- Educating caregivers and patients about the importance and benefits of availing disability certificate for moderate to severe patients. There are various Government Schemes available for CP child or adult patients.
- In India, the National Trust is a statutory body of the Ministry of Social Justice and Empowerment, Government of India, set up under the "National Trust for the Welfare of Person with Autism, Cerebral Palsy, Mental Retardation and Multiple Disabilities" Act.
- Government offers various schemes related early intervention and school readiness scheme, Day care scheme, Respite care, Group homes for adults, Health Insurance scheme, Educational scheme, provision of Aids and assistive devices etc for these Person with disability (PwD) under National trust act.






Comments